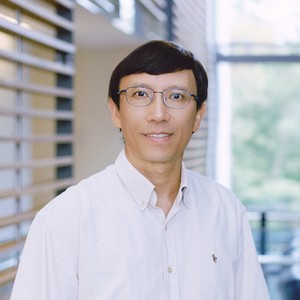
Dr. Zongchao Jia is a professor and researcher at Queen’s University who was recently funded by Cystic Fibrosis Canada for his research study, Investigation of P. aeruginosa polyphosphate kinases and their role in host cell infection for developing novel CF therapeutics. Read the article below to learn more about Dr. Jia and his contribution to cystic fibrosis research.
What are PA infections?
Pseudomonas aeruginosa (PA) is an opportunistic pathogen, meaning it’s inactive until the time is right. When the immune system is weakened, such as during burns, cuts, or chemotherapy, these bacteria seize the chance to wake up and cause damage. Although its mode of infection is comparable to other bacteria, the main problem with PA infections is that, despite typically remaining inactive, once it becomes triggered, it can be quite harmful. Additionally, most antibiotics do not work well against this infection, which is very problematic due to its high transmission and the severity of the infection.
What are some challenges or complications that are associated with this infection, especially in people living with CF?
For people with CF, the main problem is that this form of infection persistently damages the lungs in various ways. It not only weakens the lungs but reduces their capacity and degrades lung function. However, the real challenge in treating this infection is multi-drug resistance. A few years ago, WHO released a list of bacteria that urgently require new antibiotics and Pseudomonas was #2 on this list.
Once someone gets this form of infection, it's extremely difficult to cure because there are no really effective treatments. Although there are antibiotics that attempt to control it, completely getting rid of it (eradicating it) is much harder.
Can you give a brief overview of your research project?
Around 10 years ago, we focused on studying the toxin secretion system of PA. We aimed to understand how toxins are recognized and transported through this system. While searching for a way to disable it to make the bacterial stop releasing toxins, we accidentally found a compound that seemed promising, but it turned out to target the polyphosphate kinase (PPK), a type of enzyme in the bacteria, instead. By inhibiting this enzyme, we may make the bacteria less virulent without making it antibiotic resistant. This approach, known as an anti-virulence drug, shows potential but has had limited success so far. Our research aims to find and assess compounds to further develop this concept.
What inspired you to pursue research in cystic fibrosis and, more specifically, what inspired you to pursue this specific particular research project?
I think this goes back to what I consider was an accidental discovery. When we were working on the toxin secretion system, our main purpose was not to develop antibiotics, but rather to understand how the process works. By chance, we discovered the compound that inhibits the enzyme I mentioned above. Since PA is one of the most important bacteria causing lung infection in CF patients, we saw this as an opportunity to work directly in the CF research field.
In regard to CF Canada’s research priorities that were developed with the CF community, you mentioned that your work aims to help eradicate chronic PA infections. How will this be significant to the CF community?
In CF research, we know that Trikafta is making a major impact. However, some patients with rare mutations do not respond to Trikafta, and for others, serious infections have already occurred. While the modulators can manage symptoms and improve quality of life, they cannot completely eliminate PA from the lungs, which is crucial for full recovery. That’s why the development of inhibitors of these bacteria remains relevant and important. Combination therapies, like a second line of defense against persistent infections, could be essential. This kind of research is still highly relevant and much needed.
What do you see changing over the next five to 10 years?
Modulators like Trikafta have had a huge impact on the CF community, and I hope it can be further improved or perfected. In combination with a future PA inhibitor therapy, we may see that even more people with CF will live long and healthy lives. I genuinely believe that we are beginning to see the light at the end of the tunnel and I am optimistic about the work that CF researchers are doing to work toward this goal. The future is bright for cystic fibrosis research.