Dr. Gagan Gupta is a professor and researcher at Toronto Metropolitan University in the department of Chemistry & Biology. Dr. Gupta was recently funded by Cystic Fibrosis Canada for his study, Connecting CFTR interaction profiling and drug response in cellular models of human airway, receiving an early career investigator award for his work. Read below our conversation with Dr. Gupta about his work and involvement with cystic fibrosis.
Can you provide a brief overview of your research?
Every cystic fibrosis (CF) patient is unique, and the disease itself has unpredictable outcomes. As a result, their responses to treatments and the way other CF-related conditions manifest can vary greatly. My research focuses on supporting individual CF patients in creating personalized treatment plans. I envision a future of personalized medicine where patients receive slightly different medications based on the severity of their symptoms, tailoring everything specifically to their condition.
The primary goal of my research is to pave the way for this future personalized therapy. The CFTR protein normally interacts closely with many other proteins in the body. Some or many of these interactions may be disrupted in cystic fibrosis. We aim to identify the interacting partners of the defective CFTR protein in cystic fibrosis. By doing so, we can develop new tools to study these partners and better understand how CFTR functions in the cell when it’s defective. This understanding will shed light on the disease and open up new possibilities for treatment.
What are these CFTR networks and why are they such an important area for research?
A lot of these networks were previously unknown, and the ones that were known were identified using different techniques. Many of these techniques involved using cells that were already broken open, essentially using dead cells, which might have caused some interactions to be lost. However, the technique we will be using identifies these partners in living cells, using a more modern approach to discover the CFTR interactors. With this method, we are building the CFTR network and trying to comprehend how it changes in individuals with cystic fibrosis.
In addition to the significant differences we’ve noticed, we have observed that some of these networks start to function normally when modern CFTR correctors like Orkambi and Trikafta are added. This is the heart of our research, and we believe it can have a positive impact on patients today. By understanding and restoring these missing interactions, we can develop better, more personalized treatment options.
How will your research impact the population of people with CF who are currently ineligible for Trikafta, or those cases where Trikafta does not work?
Even though Trikafta has been revolutionary and has allowed patients to live close to normal lives, their recovery is still not 100%. Therefore, our goal is to achieve better treatment options for everyone.
And of course, there is still a significant portion of CF patients who don’t respond to Trikafta at all. However, much of what we do will help design improved treatments for these non-responding patients or those unable to take Trikafta.
CF Canada has a number of research priorities that were determined by the CF community. Your proposal mentioned that your research will work towards curing CF with gene or stem cell therapies and also reducing the treatment burden. Can you explain how your research will address this and why it’s an important area of focus?
In gene therapy, if we identify crucial proteins that interact with CFTR and the genes controlling them, we can figure out if CFTR responds positively to treatment or not. Then, we can work with modifier genes alongside CFTR. We may use therapies that either boost or reduce the function of those genes for specific patients. This, combined with fixing CFTR function, can improve their treatment.
Regarding stem cell therapy, I believe that gaining a deeper understanding of CFTR within the cell will lead to a more effective cure for CF, maybe even using stem cells in the future to treat patients.
Congratulations on receiving an early career investigator award. How significant do you feel it is for CF Canada to fund early career researchers like yourself?
It has been extremely important. When we started doing this work, I was really interested in this field and I wanted to make an impact. For a very long time, our work was unfunded, however we knew we were capable of making important discoveries. So, when CF Canada decided to fund us, it was a really big validation of all the effort that my students and I had put in and it really motivated us to keep going.
As an early career investigator, it's difficult to get established. So, any amount of funding that can help us retain students is very valuable to our work. It's also an important form of validation of all of the hard work that is getting put into our research. So, this funding from CF Canada was an extremely big deal for us and I think every field benefits from having good and new ideas come into it. I also feel that I have been very welcome into the CF field, as this award has also connected us into the CF network, allowing us to get advice, reagents and cell lines from people in the CF field, which is so incredibly important.
What do you see changing over the next five to 10 years for those living with cystic fibrosis?
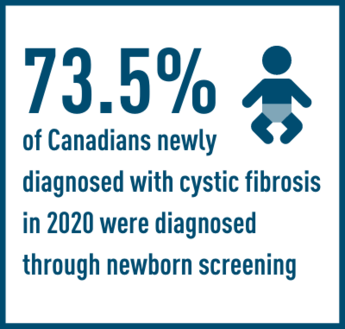
In the next five to 10 years, I think we can expect the development of next-generation modulators that will greatly impact CF patients, providing even better treatments. There will likely be more progress in addressing CF-related conditions beyond lung complications, such as GI issues and pancreatic exacerbations, with the focus on finding effective therapies. With the CF population in Canada now living longer, I think that research will also explore the health challenges faced by older CF patients. I also believe that efforts to build networks in parts of the world without extensive screening programs, like India and China, will help guide future treatments for patients worldwide.